Dysphagia is a medical term that refers to difficulty with swallowing. It’s a common complication among individuals with Parkinson’s disease, a neurodegenerative disorder that impacts the nervous system. Dysphagia can cause significant distress and discomfort, as it can impact the quality of life and increase the risk of complications, such as malnutrition, dehydration, and pneumonia.
Causes of Dysphagia in Parkinson’s Disease
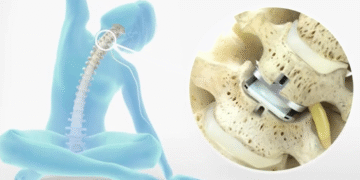
In people with Parkinson’s disease, dysphagia is mainly caused by the motor symptoms of the disease such as tremors, rigidity, bradykinesia, and postural instability. These symptoms can affect the muscles involved in swallowing, such as the tongue, throat, and esophagus, making it difficult for food and liquid to pass through the digestive tract.
In some cases, dysphagia in Parkinson’s disease may also be caused by non-motor symptoms such as cognitive impairment. This can impact the patient’s ability to coordinate their muscles and manage their swallowing reflex.
Symptoms of Dysphagia in People with Parkinson’s Disease
The symptoms of dysphagia in people with Parkinson’s disease can vary depending on the severity and stage of the condition. Some common symptoms include:
- Difficulty initiating swallowing
- Feeling of food or liquid being stuck in the throat or chest
- Choking, coughing, or gagging during or after eating or drinking
- Regurgitation of food or liquid from the esophagus
- Drooling or excess saliva production
- Weight loss or malnutrition
Diagnosis of Dysphagia with Parkinson’s Disease
Diagnosing dysphagia in somebody with Parkinson’s disease can be challenging, as the symptoms can be quite subtle and may not always appear until the later stages of the disease. However, there are several tests and procedures that may help diagnose this condition, including:
- Clinical examination: The doctor may perform a physical examination to check the patient’s ability to swallow and look for any signs of muscle weakness or dysfunction.
- Videofluoroscopy: This is a test that involves swallowing a barium-coated food or liquid while a video camera records the movement of the muscles involved in swallowing.
- Fiberoptic endoscopic evaluation of swallowing (FEES): This test involves passing a flexible endoscope through the nose and down into the throat to examine the patient’s swallowing mechanism.
Managing Dysphagia in Patients with Parkinson’s Disease
Management of dysphagia in patients with Parkinson’s disease requires a multidisciplinary approach involving neurologists, speech-language pathologists, dieticians, and occupational therapists. Some common management strategies include:
- Diet modification: The patient may need to modify their diet by eating soft foods, blending food, cutting food into small pieces, or using products like SimplyThick beverage thickening gel to make liquids easier to manage.
- Speech therapy: This involves exercises and techniques that are designed to help strengthen the muscles involved in swallowing, while also improving the patient’s ability to manage their swallowing reflex.
- Medications: A doctor may recommend certain medications to help improve the patient’s swallowing function by reducing tremors or muscle rigidity.
- Surgery: In severe cases, surgery can be carried out to implant a feeding tube or correct anatomical abnormalities that are affecting the swallowing mechanism.
Dysphagia is a common complication among patients with Parkinson’s disease, and it can have a significant impact on their quality of life. Understanding the causes, symptoms, treatment options, and management strategies is crucial for improving the patient’s overall health and wellbeing.